Smartphones Irradiate the Thyroid:
Is This a Cancer Risk?
Looking Beyond Overdiagnosis as
Tumors Continue To Surge
Thyroid cancer among women is skyrocketing all over the world. Incidence is growing faster than for any other cancer. This has been going on for a long time, and the reasons why remain elusive.
The prevailing view is that there’s been an “epidemic of diagnosis” —that is, overdiagnosis— particularly following a screening program. The tumors have always been there, the argument goes, but new and better detection tools (ultrasound, for example) have made it easier to spot small ones, many of which would likely never present a real threat. In any case, thyroid cancer is not one of the bad ones; 98-99 percent of those diagnosed survive at least five years, the highest for all cancers. Watchful waiting is often the best prescription.
The only recognized cause for thyroid cancer is ionizing radiation, with a latency of just two or three years.* Too many throat X-rays may lead to a thyroid tumor. Children exposed after the nuclear meltdown at Chernobyl suffered a “dramatic” increase in thyroid cancer, yet there was no discernible rise among adults.
In 2016, Sweden’s Michael Carlberg, a biostatistician, and Lennart Hardell, an oncologist and epidemiologist, made a case that more attention should be paid to RF/microwave radiation from cell phones. They pointed out that the antenna in smartphones is on the bottom of the phone, and, when the phone is held up to the ear, it directly irradiates the thyroid (see below).
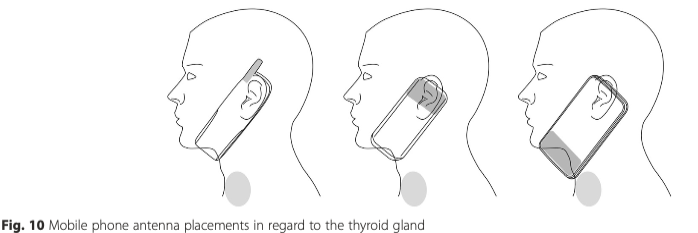
Source: Carlberg, et al., BMC Cancer, 2016
There was no follow-up until late 2018, when Yawei Zhang at the Yale School of Public Health published the first epidemiological study of its kind. She found some elevated tumor rates, but nothing significant. The study was generally regarded as an all clear.
Then last December, Zhang updated her analysis by adding genetics information to the mix. She showed that those who have variant DNA repair genes are more susceptible following prolonged use of a cell phone. For some variants, the tumor risk was some five times greater than that of those with the more common genes, a significant finding. (See: “Cell Phones and Cancer: Your Genes May Tell the Story.”)
Importantly, Zhang’s studies say little about the possible role of smartphones, since her data were collected a decade ago when the phones were relatively new to the market. Her study population would have had less thyroid exposure while on the phone because in earlier generations of phones the antenna was further away from the neck.
Tumor Incidence Still Rising in Sweden
At about the same time as Zhang’s new paper appeared in Environmental Research, the Swedish Cancer Registry released its 2018 tumor data.
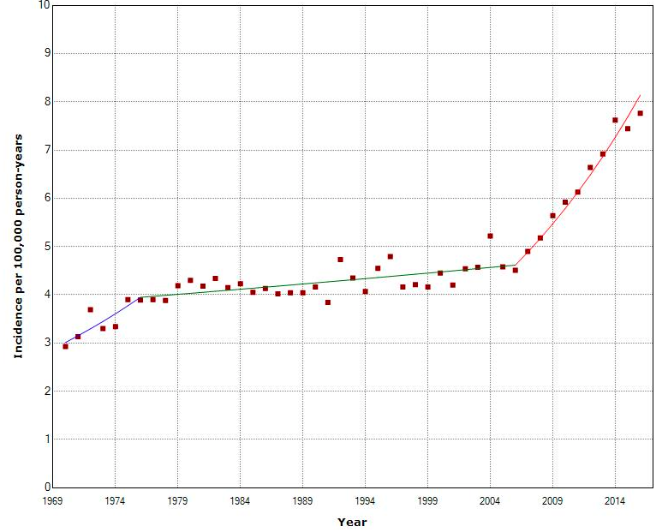
Mona Nilsson, who runs the Swedish Radiation Protection Foundation from Adelsō, not far from Stockholm, sent me an updated graph for thyroid cancer. The rate among women continues to spike. The pace appears to be rising even more sharply than when Carlberg and Hardell first expressed their concerns four years ago.
Because Nilsson had plotted the crude numbers from the registry website, I asked Alasdair Philips to graph age-standardized data to take into account any changes attributable to an aging population.‡ (Philips, who lives in Scotland, has had extensive experience analyzing brain tumor rates.) Here’s what he sent me:
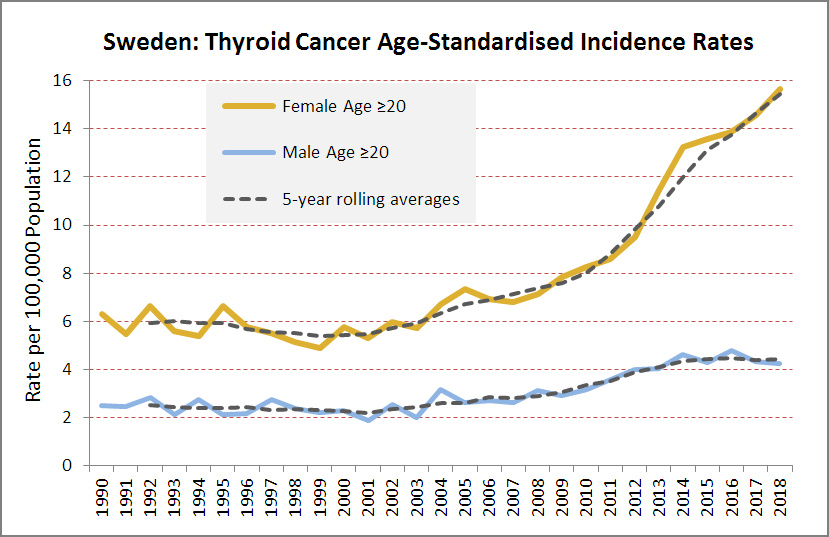 Source: Alasdair Philips for Microwave News
Source: Alasdair Philips for Microwave News
As it happens and to the surprise of many, the Swedish Cancer Registry counts each thyroid tumor as a case —not each person with thyroid tumor(s). So a person with two tumors counts as two cases. The Registry does, however, compile the latter data and presents them in a separate four-page report on the new set of statistics. These are the trends for people with thyroid cancer:
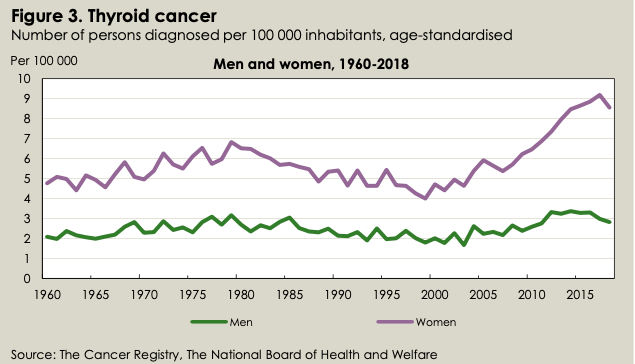 Source: Socialstyrelsen, Statistics on Cancer Incidence 2018
Source: Socialstyrelsen, Statistics on Cancer Incidence 2018
The Registry’s plot for women (top curve, above) is a bit less steep than Philips’s because the Registry includes all Swedes with thyroid tumors, not just those over 20 years old. Philips excluded those under 20 because, he told me, they rarely get thyroid cancer unless exposed in a nuclear accident.
About the dip in 2018: In its accompanying text, the Registry points out that it is due to a delay in reporting new tumors. The 2018 number will rise when the Registry updates its statistics next October. This happens every year. Take a look at the Registry’s 2016 graph below. It too has a dip, but it’s now gone and the curve has reversed direction.
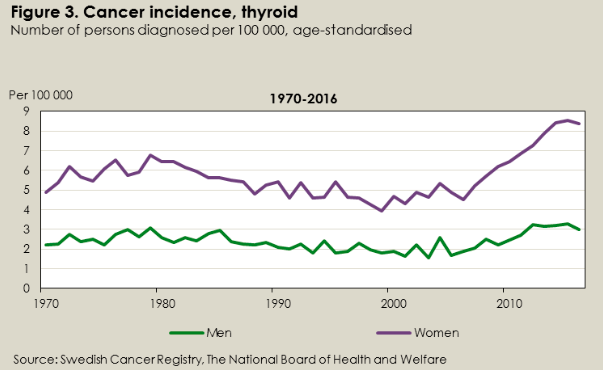 Source: Socialstyrelsen, Statistics on Cancer Incidence 2016
Source: Socialstyrelsen, Statistics on Cancer Incidence 2016
These missing cases also mean that Philips’s incidence curve will become even more striking when the Registry’s database is fully updated.
Large Tumors Keeping Pace with Smaller Ones
This year’s cancer summary features a second set of graphs:
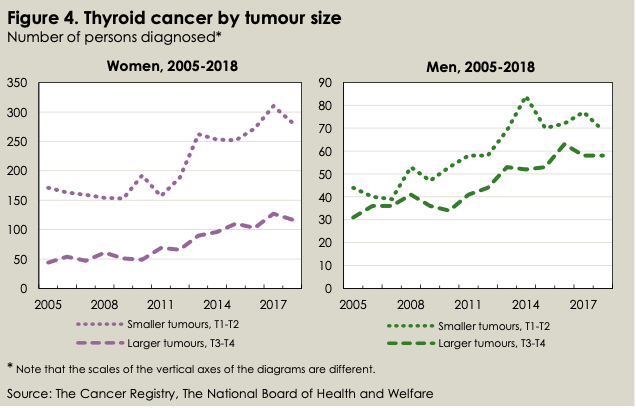
Source: Socialstyrelsen, Statistics on Cancer Incidence 2018
They show the change in incidence of small (<4cm, top curves) and large (>4cm, bottom curves) tumors between 2005 and 2018. They make the case that something more than better detection is at work.
The smaller, indolent tumors are those that may have been hidden until more sensitive diagnostic tools came into use. Detecting small tumors is widely held to account for the big rise in overall incidence. Large tumors, on the other hand, may have gone unnoticed when small, but as they grew and became more symptomatic, they would have most likely been detected. If the jump in incidence is indeed all about detection, the ratio of small to large tumors should have increased over time. But that’s not what the graphs show.
“The ratio between smaller and larger tumors has not changed between 2005 and 2018,” David Petterssen, a statistician at the Swedish National Board of Health and Welfare (Socialstyrelsen), told me in an email. This “does not speak in favor of the notion that the increased incidence would merely be a result of diagnostic intensity, i.e. increased detection of asymptomatic, non-visibly notable tumors,” he wrote. The Board oversees the Cancer Registry.
There is “evidence of a ‘real’ increase,” added Shiva Ayoubi, another statistician at the Cancer Registry. “Research is under way to find the cause of it,” Ayoubi wrote in a separate email exchange.
“Specialists in endocrine tumors in Sweden are aware of the questions the data raise,” Lars Holmberg, a professor emeritus at King’s College, London, and an advisor to the Swedish Cancer Registry, told Microwave News. “There is a need to investigate if there is a true increase in clinically relevant tumors,” he added.
Obesity as a Risk Factor
Three years ago, Cari Kitahara at the National Cancer Institute showed that improved diagnosis is not the whole story in the U.S. either. Writing in the Journal of the American Medical Association (JAMA), she reported that she can see a “true increase in the occurrence of thyroid cancer in the United States.”
Kitahara has been focusing on the risk associated with being overweight or obese. “The trends we are observing for advanced and large tumors may be (at least partly) related to changes in the prevalence of lifestyle or environmental risk factors,” she told me.
Weight gains “may have contributed importantly to the rapid rise” of the most prevalent type of thyroid tumor in the U.S. during 1995–2015, she reported in the Journal of the National Cancer Institute just a few weeks ago.
Soon afterwards, a letter appeared in JAMA showing that while the U.S. incidence of small thyroid tumors is leveling off, large ones are still rising (in this case small is 1cm or less, see below):
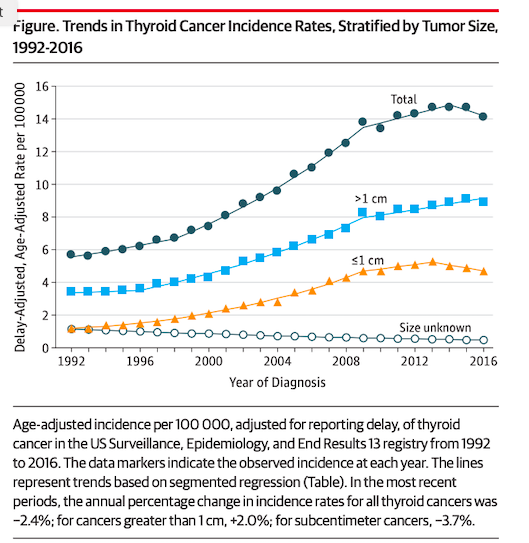 Source: JAMA, December 24-31, 2019
Source: JAMA, December 24-31, 2019
In an email exchange, I asked Kitahara how much of the jump in thyroid tumors could be attributed to being overweight or obese. “About 10-15%,” she said.
“Might RF radiation from cell phones be playing a role?” I followed up. “I think it is very unlikely,” Kitahara replied. “Currently, there is insufficient evidence of a causal link between use of cell phones and thyroid cancer risk.”
Still, Zhang at Yale SPH concludes in her most recent paper that more studies are “urgently needed” to sort out the mechanism of interaction between genetics and cell phone radiation in the development of thyroid cancer.
“Alarming” Rise in Thyroid Tumors in Sweden
Lennart Hardell also wants more research. Mona Nilsson had sent him her graph with the latest Cancer Registry data. I asked for his reaction.
“The increasing incidence of thyroid cancer is certainly alarming and cannot be explained by increased exposure to X-rays, for instance, CT of the thyroid gland, or by Chernobyl,” Hardell replied. “The dramatic increase starts in the mid-2000s and may correlate with the use of smartphones.”
He stressed that there is no screening for thyroid cancer in Sweden. The Swedish Cancer Society confirmed this for me.
“The data in the Cancer Register are not detailed enough to give good clues about the causes,” cautions Holmberg. For now, he said, “It is very difficult to speculate what the reasons for the development may be.”
Hardell and Carlberg are in the process of using the latest data to take a new look at the trends across all the Nordic countries —these include Denmark, Finland, Iceland and Norway as well as Sweden. They are using the NORDCAN database, which counts a case as a person with thyroid cancer. [Their paper has now been published, see update below.]
They shared a preliminary graph of the combined Nordic tumor data with Microwave News (see below). The rate of thyroid cancer for women across all these countries has nearly doubled since 2006 and shows no sign of slowing down.
Age-Standardized Incidence of Thyroid Cancer, Women, Nordic Countries (NORDCAN), 1970-2016
Source: M. Carlberg and L. Hardell, Personal Communication
Is There an RF/MW Link to Thyroid Cancer?
Despite substantial evidence implicating RF/microwave radiation with brain cancer, a link to cell phones has been dismissed because brain tumor rates are not rising in the general population —even though there appears to be a jump in the more aggressive type, glioblastoma, in a number of countries.
For thyroid cancer, the opposite holds. Rates are going through the roof, notably after the introduction of smartphones at the turn of the millennium. But there hasn’t been much research to test the assumption that RF/microwave radiation cannot affect thyroid tissue.
There is a significant, but largely overlooked, animal study carried out by Bill Guy at the University of Washington in the 1980s: It showed that microwaves caused many more endocrine tumors, including of the thyroid, among exposed rats. (See our 1984 cover story: “Microwaves Promote Cancer.”)
The National Toxicology Program recently refuted the orthodoxy that RF/microwaves cannot cause cancer. Will history repeat with smartphones and thyroid cancer?
Carlberg-Hardell Paper on Thyroid Cancer in Nordic Countries Published
December 7, 2020
The Carlberg-Hardell analysis of thyroid incidence in Nordic countries was posted today. (It is open access). They conclude:
“We postulate that RF radiation is a causative factor for the increasing thyroid cancer incidence.”
Swedish Expert Group Calls for More Research on Mobile Phones and Thyroid Cancer
April 28, 2021
In a report issued today, the Scientific Council on EMFs of the Swedish Radiation Safety Authority (SSM) recommended more research to investigate the possible link between the use of mobile phones and thyroid cancer.
Bluetooth Headset and Thyroid Nodules
June 30, 2024
New paper:
“Prolonged & frequent use of Bluetooth headphones may be associated with an increased risk of developing thyroid nodules, potentially linked to cumulative effects of NIR emitted by headphones on the thyroid gland.”
From China and Malaysia. Open access.
__________________
* This is a minimum estimate from the CDC. A 2017 review puts the latency at 5 to 10 years.
‡ Standardizing incidence data adjusts for changes in the age distribution of the population. It is particularly important for those cancers which become more prevalent as people age: An increase may simply reflect that there are more older people rather than a true increase in incidence. Women are more likely to be diagnosed with thyroid cancer in their 40s and 50s, according to the American Cancer Society, while men are usually diagnosed in their 60s and 70s. The ACS also states: “For unclear reasons thyroid cancers (like almost all diseases of the thyroid) occur about three times more often in women than in men.”
